Background/Purpose: Obesity and pro-inflammatory cytokines produced by adipocytes have been linked to many outcomes including disease severity, treatment response, and disease progression in several autoimmune conditions [1]. However, there is a paucity of literature describing the relationship between adiposity and outcomes in juvenile dermatomyositis (JDM). We sought to characterize and evaluate the impact of adiposity among JDM patients.
Methods: This single center retrospective study included patients diagnosed with JDM between 2008-2018. Patients diagnosed at an outside institution without known baseline body mass index (BMI) or previously treated with systemic medications were excluded. The cohort was divided according to BMI categories, as defined by the US Centers for Disease Control and Prevention (CDC) BMI-for-age growth chart (overweight defined as BMI ≥ 85th percentile and < 95th percentile; obesity defined as BMI ≥ sex-specific 95th percentile). Data extracted from chart review included demographics and clinical characteristics (including clinical features, laboratory data, Childhood Myositis Assessment Scale (CMAS), and physician global scale of overall disease activity). Differences between groups were assessed using chi-square test, Fisher’s exact test, and Mann-Whitney test, as appropriate.
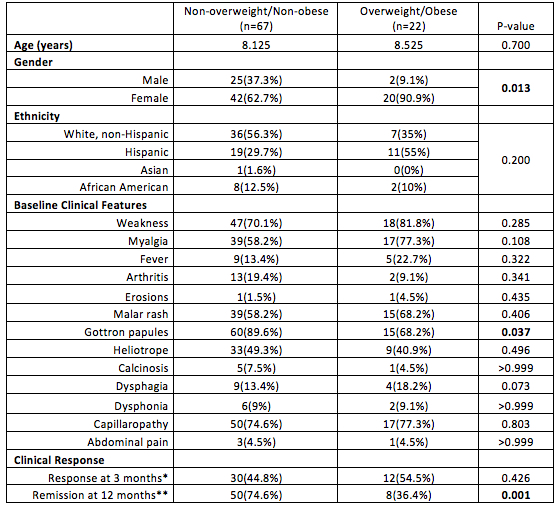
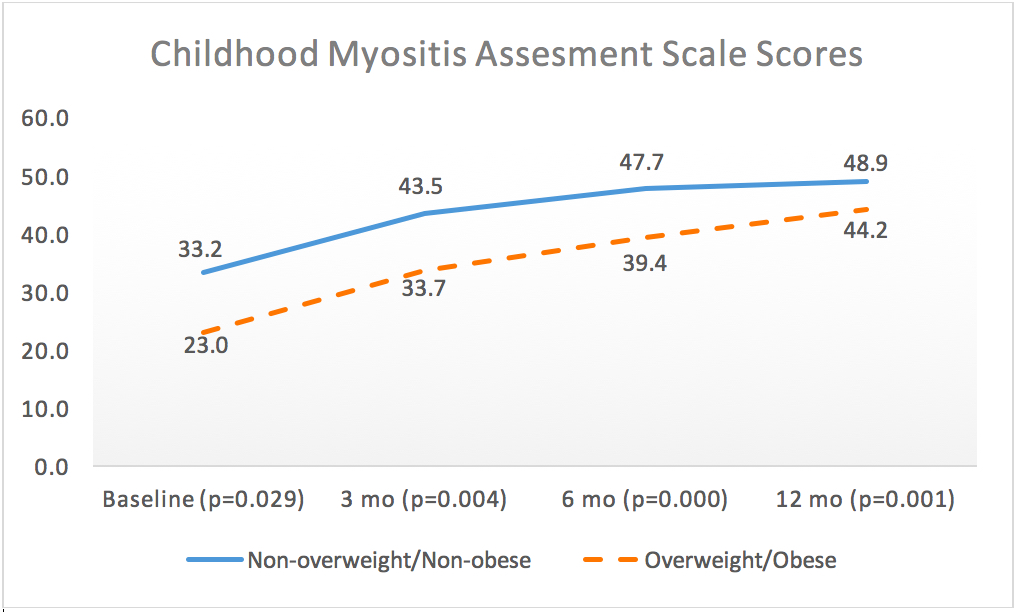
Results: Eighty-nine patients were included in the analysis with 67 (75%) with a BMI < 85th percentile and 22 (25%) with a BMI ≥ 85th percentile. At baseline, there was no statistical difference between group in terms of age of diagnosis (mean age = 8.22 years), ethnicity, and clinical features except the non-overweight/non-obese group had more Gottron papules (p=0.037) and the overweight/obese group were predominantly female (p=0.013) (Table 1). However, at baseline the overweight/obese group had significantly higher creatinine kinase (p=0.015) and ALT (p=0.050) and scored lower on the CMAS (p=0.029). Lower CMAS scores also persisted in the overweight/obese group at the 3 month, 6 month, and 12 month visits (Figure 1). There was a significant trend towards higher LDH and aldolase in the overweight/obese group at subsequent visits (Table 2). There was no difference in response to treatment at 3 months. Yet, fewer patients in the overweight/obese group achieved clinical remission at 12 months (36.4% vs. 74.6%, p=0.001).
Conclusion: In this descriptive analysis of a cohort from a single center, higher adiposity at time of diagnosis among JDM patients is associated with higher muscle enzyme and lower CMAS scores. Excess adiposity also appears to negatively impact the disease course and is correlated with lower rates of clinical remission at 12 months from diagnosis.
References: [1] Versini M, Jeandel PY, Rosenthal E, Shoenfeld Y. Obesity in autoimmune diseases: not a passive bystander. Autoimmun Rev. 2014; 13(9):981-1000.
*Response at 3 months was defined as response to glucocorticoid and/or 1 other immunosuppressive or immunomodulator.
**Remission at 12 months was defined according to the Pediatric Rheumatology International Trials Organization (PRINTO) criteria for clinically inactive disease in JDM (meeting at least 3 out 4 of the following: CK ≤ 150, CMAS 48, manual muscle testing (MMT) ≥ 78, and physician global assessment ≤ 0.2). In instances where a CMAS or manual muscle testing was not performed (i.e. due to age), inactive disease criteria also included lack of active clinical disease features including no active skin lesions.
The post Discovering the Implications of Adiposity in Juvenile Dermatomyositis appeared first on ACR Meeting Abstracts.