Background/Purpose: JIA – associated uveitis (JIA-U) accounts for 20-40% of childhood noninfectious uveitis and affects 10-20% of patients with JIA. Its chronic course is often painless and insidious, and early treatment is crucial to prevent ocular damage and blindness. Screening guidelines have been established to detect uveitis, but even after treatment, patients are at risk of recurrence1. It is not known whether children with JIA-U should be evaluated for active uveitis at the time of detected arthritis flare. This is the first large, systematic evaluation of arthritis activity as it temporally relates to uveitis activity within a well-defined time period over the JIA-U disease course.
Methods: This is a retrospective, single-center, longitudinal cohort study using medical record
data of patients with JIA-U. Uveitis and arthritis data were collected longitudinally from 7/2013 – 12/2019. Presence of uveitis was defined by Standardization of Uveitis Nomenclature2; arthritis activity was defined by presence of arthritis in >0 joints. Repeated measure logistic regression was used to evaluate for an association between uveitis activity within 45 days before and after any arthritis activity. Correction for individual variables was also performed.
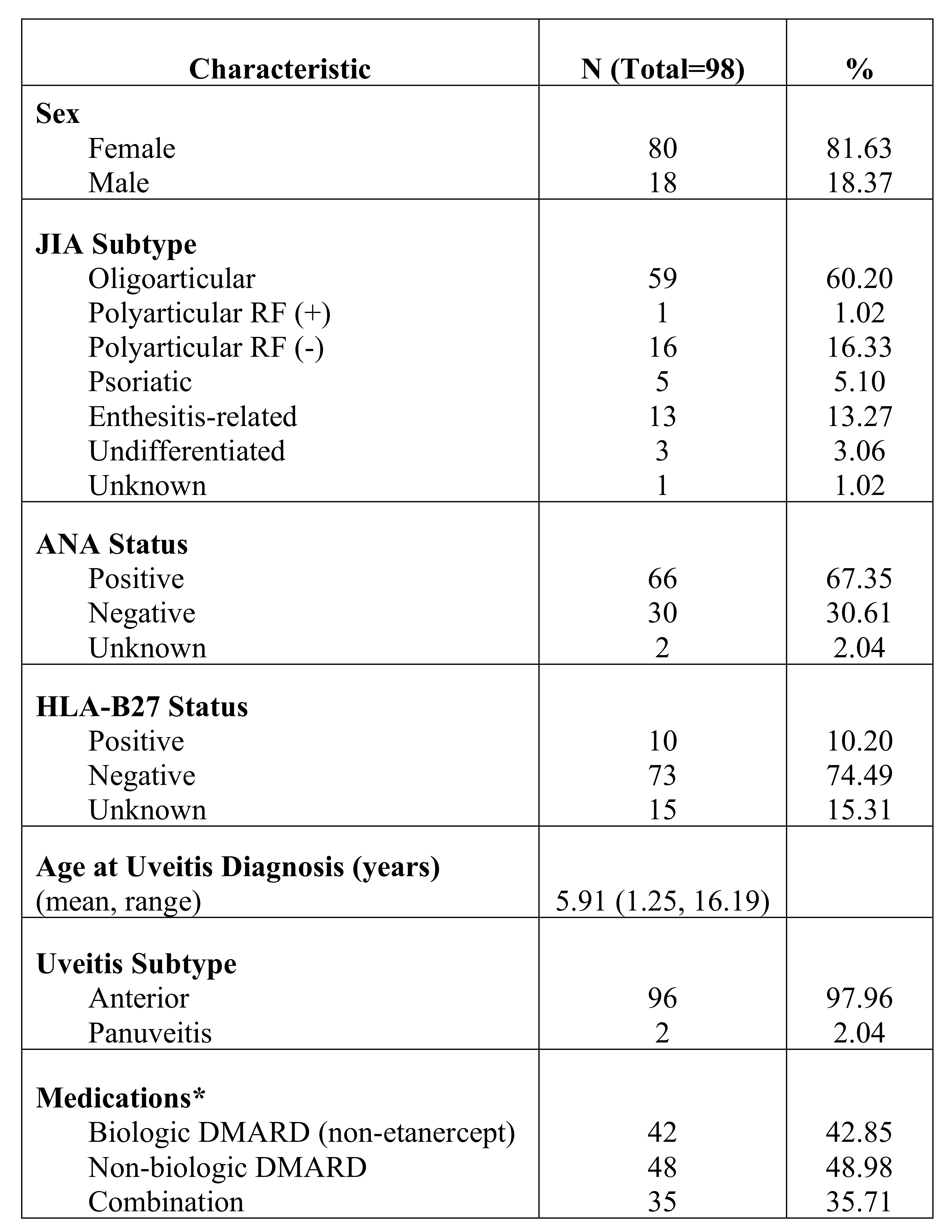
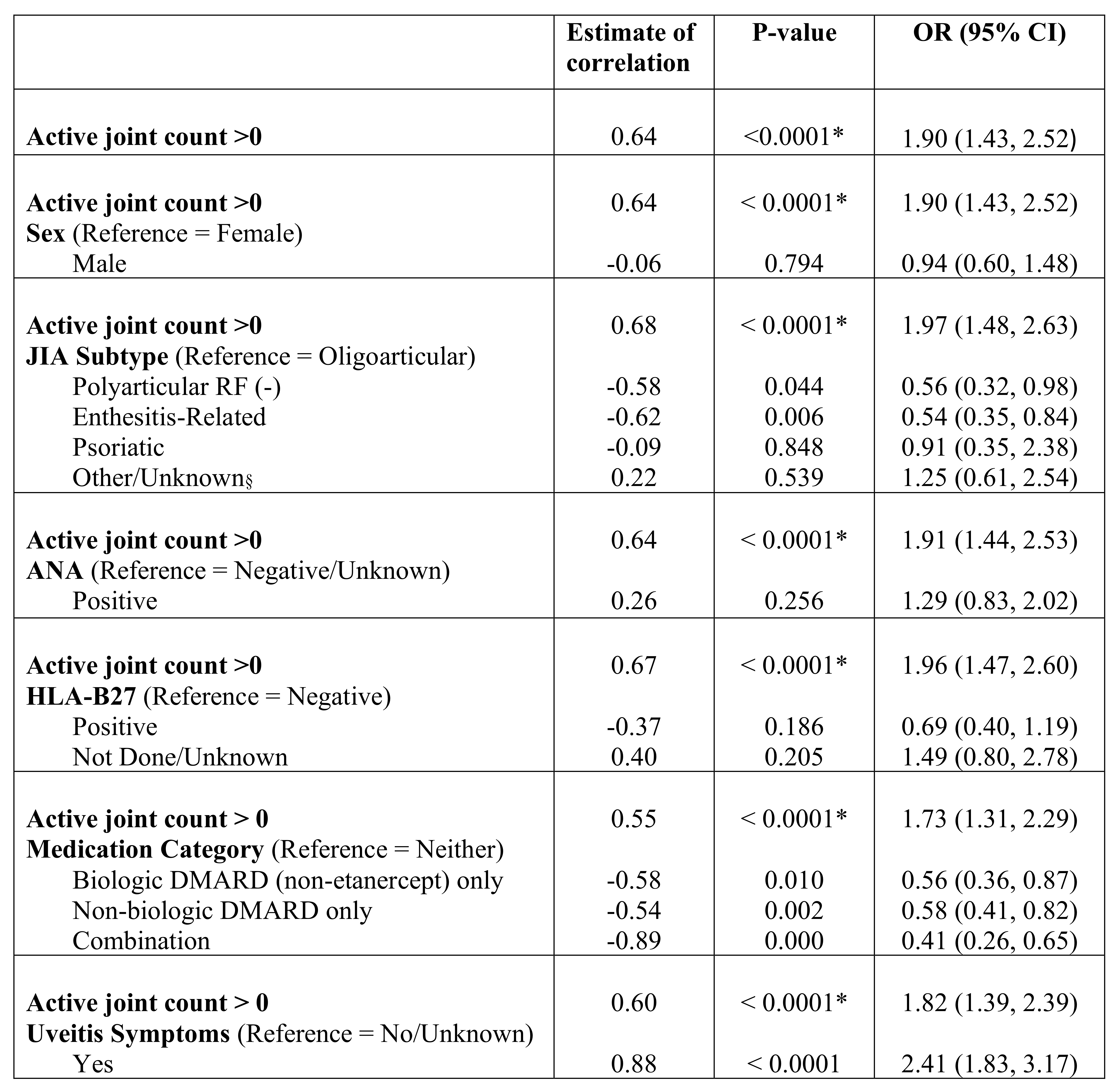
Results: Ninety eight patients with JIA-U were included; 96 (97.9%) had anterior uveitis and 59 (60.2%) were oligoarticular subtype. There were 2765 ophthalmology and rheumatology visits across the cohort. 40 (41%) patients had 137 visits with active uveitis within 45 days of any arthritis activity, yielding a positive temporal association between arthritis and uveitis activity, odds ratio (OR) 1.90 [95% confidence interval (CI): 1.43, 2.52; p< 0.0001]. The oligoarticular subtype had the strongest association, OR 1.50 [95% CI: 1.08-], 2.09; p=0.015]. Sex, ANA status, and HLA-B27 status did not significantly affect the association. Treatment with biologic and non-biologic DMARDs alone and in combination decreased the association between arthritis and uveitis activity, but the overall estimated correlation remained significant, OR 1.73 [95% CI: 1.31, 2.29; p< 0.0001].
Conclusion: In patients with JIA-U, there is a positive association between arthritis activity and uveitis activity within a 45-day period, that is strongest in the oligoarticular subtype. This suggests that joint or eye disease flare should prompt referral to the ophthalmologist or rheumatologist, respectively. Biologic and non-biologic DMARD mono- and dual therapy mitigates, but does not eliminate, this association.
1. Heiligenhaus A, Niewerth M, Ganser G, Heinz C, Minden K, German Uveitis in Childhood Study G. Prevalence and complications of uveitis in juvenile idiopathic arthritis in a population-based nation-wide study in Germany: suggested modification of the current screening guidelines. Rheumatology (Oxford). 2007;46(6):1015-1019.
2. Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature Working G. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509-516.
*Number of patients with at least 1 visit on biologic DMARD (non_etanercept) alone, non_biologic DMARD alone, or both concurrently.
* Indicates statistical significance (p<0.05) of association overall and corrected for individual variables.
§ Includes polyarticular RF (+) and undifferentiated subtypes.
The post Evaluating the Relationship Between Juvenile Idiopathic Arthritis Disease Activity and Uveitis Activity: A Retrospective Analysis appeared first on ACR Meeting Abstracts.